Thyroid hormone and brain function
T3 is critical to the communication that goes on in the brains of adults and children
[Adapted from my 2006 book, Rhythms of Life, with selected references]1
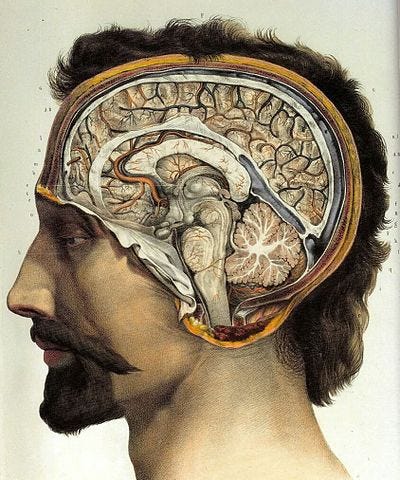
Thyroid hormone, specifically T3, is essential for day-to-day brain function. T3 is critical to the communication that goes on in the brain, in part because it has a fundamental role in controlling brain-specific genes, but also because it’s required for brain synapses to function properly.2
The essential fatty acid known as DHA (docosahexaenoic acid) is also necessary for brain development and brain function because it’s required for the production of transthyretin—the hormone transport molecule that moves thyroid hormone around the brain.3
In other words, if a portion of the brain doesn’t receive the thyroid hormone it needs because the transport mechanism isn’t working efficiently, synapse and gene function will be compromised. This relationship between thyroid hormone and DHA means that sufficient amounts of the essential fatty acid and T3 must be present for optimal brain function. Because most brain activity specifically requires T3, a critical aspect of brain function is local tissue conversion of T4 to T3, which is accomplished by a specific enzyme (D2 deiodinase).
[As discussed previously, during fetal development, severely deficient levels of thyroid hormone supplied by the maternal system (most commonly seen in cases of acute iodine deficiency) can cause the profound form of mental retardation known as cretinism. However, even mild fetal insufficiency can cause detectable brain defects, including deafness.4
In some cases, particularly in deafness, these defects can result from localized rather than general T3 deficiency, because the cochlea requires specific amounts of T3 at specific times for proper formation.5 In other words, deafness and perhaps other defects can be caused by insufficient amounts of the enzyme D2 deiodinase that are needed at specific times during fetal development.]
Thyroid disorders, but particularly low thyroid production—hypothyroidism—can result in a number of symptoms that indicate impaired brain function, including depression, poor memory, inability to concentrate, mood swings, sleep disturbances, and anxiety.
These symptoms in peri-menopausal women are often blamed on declining levels of estrogen. I’ve been there, and believe me when I tell you, these are not trivial inconveniences: they are changes that profoundly impact a woman’s ability to function as she’s been used to doing her entire life.
However, because thyroid function is well known to decline with age in all animals (including humans) and to impact a wide variety of body functions (including temperature regulation, general metabolism, and heart function, among others), these symptoms are far more likely to be the ultimate result of age-associated TH reductions that also impact changes in estrogen production.
In other words, age-related TH declines are the problem: estrogen declines are as much of a symptom as the brain fog and depression.
Much more on these issues in future posts because they are the core of what I’d like to explore here.
But to further whet your appetite, hypothyroidism has also been strongly linked to hyperactivity disorders in children, to postpartum depression and to some kinds of post-traumatic stress disorder (particularly where the situation involves a “sit and endure” type of stress rather than a “fight and run for your life” type).6
People do not often die of these disorders but they are very often rendered under-productive or even non-productive.7
That’s because modern humans have a low tolerance to fluctuations in thyroid hormone levels: either too much (hyperthyroidism) or too little (hypothyroidism) makes us decidedly ill, although hypothyroidism is by far the most common.
This situation is almost certainly a result of our evolutionary history, so in future posts I’ll lay out how this all may have unfolded from a perspective of changing TH metabolism in our ancestors: the conundrum of bipedalism, changes in diets as environments changed, increased brain size over time, and the use of fire for cooking (among others).
These are the issues that make evolution personal, by which I mean that not until we understand precisely how humans developed into the animal species we have become—just as wolves became dogs—can we expect new and significant insights into some of the debilitating health problems that continue to plague us, many of which seem to revolve around TH metabolism.
Crockford, S.J. (2006). Rhythms of Life: Thyroid Hormone and the Origin of Species. Trafford, Victoria.
Henley, W.N. and Koehnle, T.J. (1997). Thyroid hormones and the treatment of depression: an example of basic hormonal actions in the mature mammalian brain. Synapse 27, 36-44. https://doi.org/10.1002/(SICI)1098-2396(199709)27:1<36::AID-SYN4>3.0.CO;2-E
Jones, S.A., Thoemke, K.R. and Anderson, G.W. (2005). The role of thyroid hormone in fetal and neonatal brain development. Current Opinion in Endocrinology and Diabetes 12, 10-16.
Episkopou, F., Maeda, S., Nishiguchi, S., et al. (1993). Disruption of the transthyretin gene results in mice with depressed levels of plasma retinol and thyroid hormone. Proceedings of the National Academy of Sciences USA 90, 2375-2379.
Horrobin, D. and Bennett, C.N. (1999). Depression and bipolar disorder: relationships to impaired fatty acid and phospholipids metabolism and to diabetes, cardiovascular disease, immunological abnormalities, cancer, aging and osteoporosis: possible candidate genes. Prostaglandins Leukotines & Essential Fatty Acids 60, 111-167. https://doi.org/10.1054/plef.1999.0037
Kitajka, K., Puskas, L.G., Zvara, A., et al. (2002). The role of n-3 polyunsaturated fatty acids in brain: modulation of rat brain gene expression by dietary n-3 fatty acids. Proceedings of the National Academy of Sciences USA 99, 2619-2624.
Geelhoed, G.W. (1999). Metabolic maladaptation: individual and social consequences of medical intervention in correcting endemic hypothyroidism. Nutrition 15, 908-932. https://doi.org/10.1016/S0899-9007(98)00123-3
Ng, L., Goodyear, R.J., Woods, C.A., et al. (2004). Hearing loss and retarded cochlear development in mice lacking type 2 iodothyronine deiodinase. Proceedings of the National Academy of Sciences USA 101(10), 3474-3479.
Hauser, P., Soler, R., Brucker-Davis, F. and Weintrub, B.D. (1997). Thyroid hormones correlate with symptoms of hyperactivity but not inattention in attention deficit hyperactivity disorder. International Journal of Psychological and Neurological Endocrinology 22, 107-114. https://doi.org/10.1016/S0306-4530(96)00043-1
Vermiglio, F., Lo Presti, V.P. Moleti, M., et al. (2004). Attention deficit and hyperactivity disorders in offspring of mothers exposed to mild-moderate iodine deficiency: a possible novel iodine deficiency disorder in developed countries. Journal of Clinical Endocrinology & Metabolism 89(12), 6054-6060. https://doi.org/10.1210/jc.2004-0571
Othman, S., Philips, D.I.W., Parkes, A.B., et al. (1990). A long term follow up of postpartum thyroiditis. Clinical Endocrinology 32, 559-564. https://doi.org/10.1111/j.1365-2265.1990.tb00898.x
Kuijpens, J.I., Vader, H.L., Drexhage, H.A., et al. (2001). Thyroid peroxidase antibodies during gestation are a marker for subsequent depression postpartum. European Journal of Endocrinology 145, 579-584.
Baumgartner, A., Hiedra, L., Pinna, G., et al. (1998). Rat brain type II 5’-iodothyronine deiodinase activity is extremely sensitive to stress. Journal of Neurochemistry 71, 817-826.
O’Connor, T.M., O’Halloran, D.J. and Shanahan, F. (2000). The stress response and the hypothalamic-pituitary-adrenal axis: from molecule to melancholia. Quarterly Journal of Medicine 93, 323-333. https://doi.org/10.1093/qjmed/93.6.323
Cudd, T.A., Chen, W-J. A. and West, R.W. (2002). Fetal and maternal thyroid hormone responses to ethanol exposure during the third trimester equivalent of gestation in sheep. Alcoholism: Clinical and Experimental Research 26(1), 53-58.
Canaris, G.J., Manowitz, N.R., Mayor, G. and Ridgeway, E.C. (2000). The Colorado thyroid disease prevalence study. Archive of Internal Medicine 160, 526-534. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/415184
Roberts, C.G.P. and Ladenson, P.W. (2004). Hypothyroidism. Lancet 363, 793-803.
Weetman, A.P. (1997). Hypothyroidism: screening and subclinical disease. British Medical Journal 314, 1175-1178. https://doi.org/10.1136/bmj.314.7088.1175